Spine Surgeries
Spine Surgeries

Spine Surgeries
 SPINAL CURVES
SPINAL CURVES
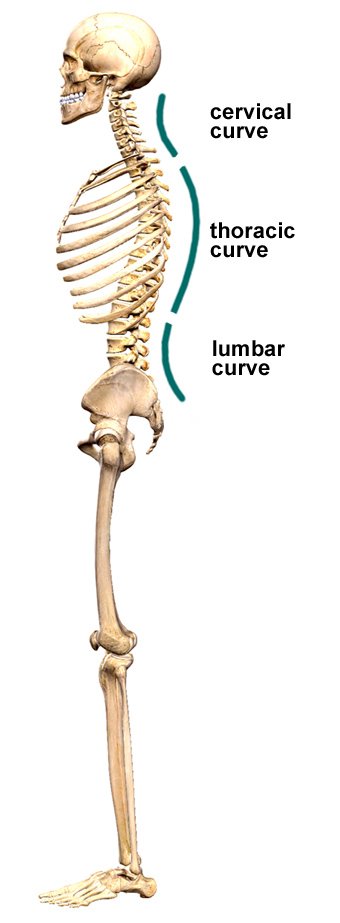
- An Abnormal Curve Of The Lumbar Spine Is Lordosis, Also Called Sway Back.
- An Abnormal Curve Of The Thoracic Spine Is Kyphosis, Also Called Hunchback.
- An Abnormal Curve From Side-To-Side Is Called Scoliosis.
 MUSCLES
MUSCLES

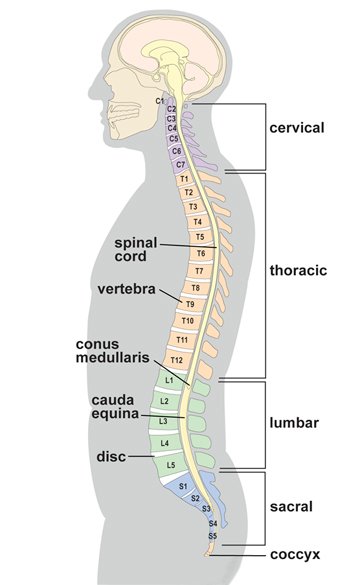
 VERTEBRAE
VERTEBRAE

Vertebrae
Cervical (neck)

- A drum-shaped body designed to bear weight and withstand compression (purple)
- An arch-shaped bone that protects the spinal cord (green) Star-shaped processes designed as outriggers for muscle attachment (tan)
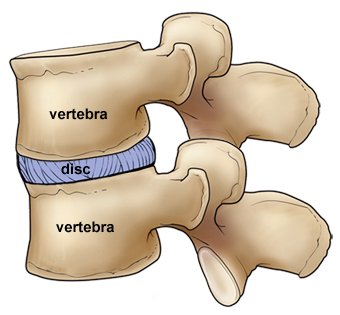
 INTERVERTEBRAL DISCS
INTERVERTEBRAL DISCS

 VERTEBRAL ARCH & SPINAL CANAL
VERTEBRAL ARCH & SPINAL CANAL


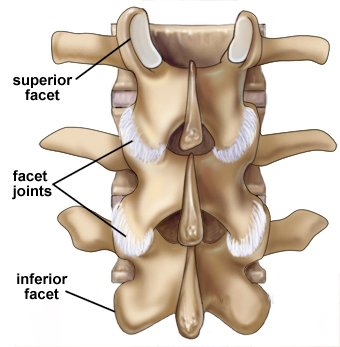
Facet joints

Ligaments
 SPINAL CORD
SPINAL CORD

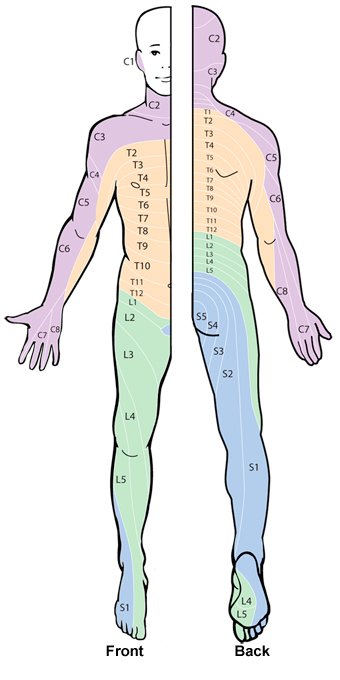
 SPINAL NERVES
SPINAL NERVES
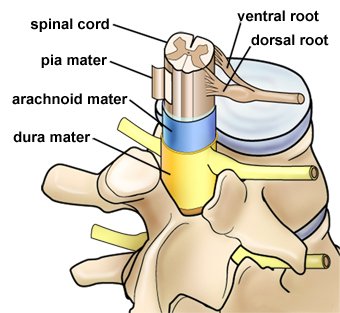

 COVERINGS & SPACES
COVERINGS & SPACES

 ENDOSCOPIC SPINE SURGERY
ENDOSCOPIC SPINE SURGERY
HOW IS LASER BACK SURGERY DIFFERENT?

Traditional

MISS

Laser
 What to expect
What to expect When pressure is placed on a nerve, it can lead to pain and discomfort.
In the spine, things like a herniated disc or a bone spur can often cause compression. An example of one such condition is sciatica, where the sciatic nerve becomes pinched, leading to pain in the lower back and leg.
Lasers can be used to help decompress the nerve, with the aim of relieving pain. This is done under local anesthesia, which means that the skin and surrounding muscles of your back will be numbed to pain. You may also be sedated for the procedure.
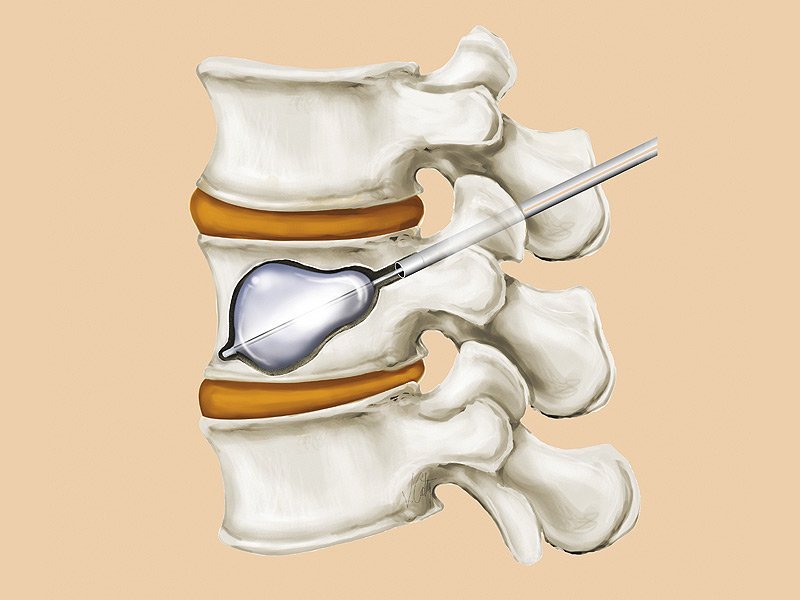
One of the more well-studied methods of laser back surgery is called percutaneous laser disc decompression (PLDD). This procedure uses a laser to remove disc tissue that may be causing nerve compression and pain.
During PLDD, a small probe containing a laser is passed into the core of the affected disc. This is accomplished with the help of imaging technology. Then, the energy from the laser is used to carefully remove tissue that may be pressing on the nerve.
 Benefits
Benefits The benefits of laser back surgery are that it’s less invasive than the traditional approach to back surgery. Additionally, it can be performed in an outpatient setting under local anesthesia. In many ways, it’s very similar to MISS.
There’s a limited amount of information regarding the overall effectiveness of laser back surgery in comparison to other methods.
One 2017 studyTrusted Source compared PLDD to another surgical approach called microdiscectomy. Investigators found that both procedures had a similar outcome over a two-year recovery period.
However, it should be noted that when discussing PLDD, the researchers included additional follow-up surgery after PLDD as part of a normal outcome.
 What is the procedure and follow-up
What is the procedure and follow-up Laser back surgery isn’t recommended for some conditions, such as degenerative spine diseases. Additionally, more complex or complicated conditions will often require a more traditional surgical approach.
One of the drawbacks to laser back surgery is that you could need an additional surgery for your condition. A 2015 studyTrusted Source found that microdiscectomy had a lower number of reoperations required compared to PLDD.
Additionally, a 2017 meta-analysis of seven different surgeries for herniated discs in the lumbar region found that PLDD ranked among the worst based off of success rate, and it was in the middle for reoperation rate.
 Side effects
Side effects Every procedure can have potential side effects or complications. This is also true for laser back surgery.
One of the main potential complications from laser back surgery is damage to the surrounding tissue. Because a laser is used for the procedure, heat damage can occur to surrounding nerves, bone, and cartilage.
Another possible complication is infection. This can occur during the placement of the probe if proper sanitization procedures aren’t followed. In some cases, you may be provided with prophylactic antibiotics to help prevent an infection.
 Recovery time
Recovery timeRecovery time can vary by individual and the specific procedure performed. Some people may be able to return to normal activities relatively quickly, while others may require more time. How does laser back surgery compare to other types of back surgery?
Having a traditional back surgery requires a hospital stay after the procedure, and recovery may take many weeks. According to the Johns Hopkins Spine Service, people undergoing traditional spine surgery should expect to miss 8 to 12 weeks of work.
In contrast, MISS is often performed as an outpatient procedure, meaning that you can go home the same day. Generally speaking, people who’ve undergone MISS may return to work in around six weeks.
You may have read that laser back surgery has a faster recovery than other procedures. However, there’s actually been very little research into how the recovery time compares.
In fact, the 2015 studyTrusted Source discussed above found that recovery from microdiscectomy was faster than for PLDD.
 GET ANSWERS FROM A DOCTOR IN MINUTES, ANYTIME
GET ANSWERS FROM A DOCTOR IN MINUTES, ANYTIME
Have medical questions? Connect with a board-certified, experienced doctor online or by phone. Pediatricians and other specialists available 24/7.

COST

ALTERNATIVE TREATMENTS

MEDICATIONS
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- muscle relaxants
- opioid pain relievers (for a very short period of time only)
- tricyclic antidepressants anti-seizure drugs

STEROID INJECTIONS

PHYSICAL THERAPY
AT-HOME CARE
 THE BOTTOM LINE
THE BOTTOM LINE

 KYPHOPLASTY
KYPHOPLASTY
What is kyphoplasty?
 CANDIDATES FOR KYPHOPLASTY OR VERTEBROPLASTY
CANDIDATES FOR KYPHOPLASTY OR VERTEBROPLASTY

 WHAT HAPPENS BEFORE AND DURING THE PROCEDURES
WHAT HAPPENS BEFORE AND DURING THE PROCEDURES


